
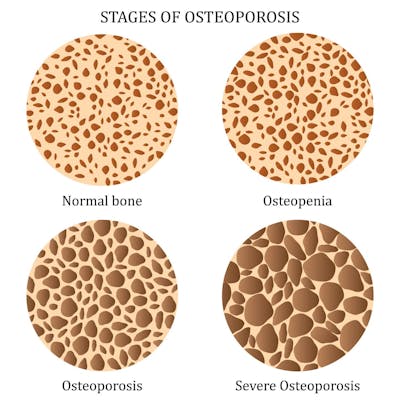
We help adults diagnosed with osteoporosis or osteopenia manage their bone health.
Osteoporosis is a bone disorder that causes bones to become weak and porous to the point of breaking easily. Bones may break from a fall or, in serious cases, even from mild stresses such as bending over or sneezing. Osteoporosis-related fractures most commonly occur in the hip, wrist, or spine.
Osteopenia or low bone density, is when bones are weaker than normal, but not so weak that they break easily, as with osteoporosis.

According to the National Osteoporosis Foundation, studies show nearly 80% of older Americans who break a bone are not tested or treated for osteoporosis.
Osteoporosis is often called the “silent disease”, because there is no pain in the early stages of bone loss. Eventually, you might notice:
- A loss of height
- A stooped posture
- A bone that breaks much more easily than expected
- Back pain caused by a broken bone in your spine
People with osteoporosis can have a broken bone in their back with only mild pain or no symptoms at all.
If you have osteoporosis, protecting your bones from breaking becomes crucial. You should avoid positions and movements that cause bones to break more easily. Avoid a slumped, head-forward position while reading and sitting at the computer, or reaching too high or too far in front of you when doing chores and yard work. A physical therapist can teach you how to improve and maintain your best body position.

Exercise has been shown to improve bone mineral density, BUT all exercises are not equally effective in managing osteoporosis and some may even be harmful if you have low bone density.

A physical therapist is the ideal healthcare provider to teach you how to exercise for improving your bone mass while avoiding exercises that may be harmful to those with osteoporosis. Weight-bearing exercises like walking, jogging, squats, and lunges, help build bone.
Strengthening exercises also help build strong bones. However, those requiring bending forward should be avoided, because they increase risk of spinal fractures. These exercises are some we are often trained to think are good for our core such as abdominal crunches, sit-ups, toe touches, and even many pilates and yoga exercises.
A physical therapist can help you by teaching you individualized exercises that are safe and effective and can make sure you are doing them correctly.
It is important for you to improve your balance and mobility as much as possible to help you avoid falls and the fractures that may accompany them.
Osteoporosis treatment may include medication and/or supplementation with calcium and vitamin D as needed. You should talk to your healthcare provider about whether you need medication at this time.

Our physical therapists work with you to adjust your posture, habits, diet and exercise routine to strengthen your bones and decrease your risk of fracture.
Our knowledgeable and caring therapists are here to help.
Read More About Osteoporosis
Causes
Bone is living tissue that is constantly being broken down and replaced. When you're young, your body makes new bone faster than it breaks down old bone and your bone mass increases. You develop what is known as "peak bone mass" between the ages of 25-30. After this timeframe, you break down bone at a faster rate than you build it. After menopause the rate increases dramatically. Studies show women lose up to 20 percent of their bone density in the five-to-seven years after menopause. The more bone mass you attained in your youth, the more bone you have "in the bank" and the less likely you are to develop osteoporosis or osteopenia as you age.
Although peak bone mass has genetic and ethnic influences, there are actions every person can take to maximize bone density and strength.
Diagnosis
The gold standard in the diagnosis of osteoporosis is to assess a person's bone mineral density using a DXA scan.
The national osteoporosis foundation (NOF) recommends testing for
- Women over 65 and younger women who have risk factors
- Men over 70 and younger men who have risk factors
- Anyone who breaks a bone in their spine from low impact
- Anyone with height loss of ½ inch or more within one year or total height loss of 1½ inches in a lifetime
If you suspect you have osteoporosis or osteopenia, ask your doctor if it's time for a DXA scan to test your bone mineral density.
Who is at the greatest risk for osteoporosis?
- Women over 50, especially Caucasian or Asian women with reduced estrogen after menopause
- Men over 70, or younger men with reduced levels of testosterone
- Small-framed people with low body weight
- Those with a family history, sedentary lifestyle, or who smoke or used to smoke
- Those with a diet low in calcium and vitamin D
- Those who drink more than 2-3 alcoholic or caffeinated drinks per day
- Those who take steroids or certain cancer medications
- Those with autoimmune, digestive, or untreated hormonal disorders
Calculate your risk using the FRAX
The Fracture Risk Assessment Tool (FRAX tool) is a tool commonly used to guide treatment for osteoporosis or osteopenia. To calculate your risk using the FRAX calculation tool go to https://www.sheffield.ac.uk/FRAX/tool.aspx?country=9
What else can I do to improve my bone health?
To slow or stop the loss of bone
- Exercise regularly.
- Eat a healthy diet with sufficient calcium and vitamin D. Leafy green vegetables, fish, and low-fat dairy products are good sources.
- Avoid smoking, excessive alcohol, caffeine, cola drinks, salt, and processed foods.
- Review your medications with your doctor to limit those that may reduce bone density.


