Have you experienced any of these common vestibular symptoms?
- Do you feel like objects in the room are spinning?
- Do you feel unsteady, off balance, or lightheaded?
- Do you become dizzy when you turn your head?
- Is it difficult to see clearly when driving or when you turn your head quickly.
- Do you become dizzy when lying down in bed, siting up, standing up or rolling over?
- Is it difficult to walk in the dark?
- Does looking up at a high shelf make you dizzy?
- Do you veer or feel like you are veering to the left or right when walking?
- Is it difficult to walk in grocery stores or areas with crowds or busy visual environments?
- Have you noticed a decline in your hearing or experience buzzing or ringing in your ears?
Where to go to get diagnosed and treated for vertigo, dizziness or balance problems?

Mary Nalls MPT, has taken extensive post graduate courses in vestibular rehabilitation and has passed Emory University’s Competency Based Vestibular exam..
First visit your doctor for appropriate evaluation and testing. Your family doctor may be able to evaluate your condition or they may refer you to a specialist who is specifically educated in vestibular dysfunctions. Doctors such as a otolaryngologist, otologist, neurologist, neurologist, otoneurologist, neuro-opthalmologist, ear nose and throat doctor (ENT) or a psychiatrist are a few that may specialize in vestibular dysfunction. Their evaluation may include a thorough subjective history and clinical exam or they may also order specialized diagnostic testing. Once properly diagnosed they may refer you to a physical therapist for treatment. Not all physical therapists are trained in this area so you must first ask if they have had specialized training in vestibular rehabilitation.
Finding Medical Help and Support:
If you would like help in finding a doctor or health care provider who specializes in vestibular disorders, or if you need a second opinion, additional diagnostics or testing of vestibular function ask your family doctor for a recommendation, or visit the Vestibular Disorders Association website:www.https://vestibular.org/finding-help-support. Or the American Physical Therapy Association Neurology Section’s website: https://www.neuropt.org/consumer-info/neurologic-disorders-index/vestibular-disorders-dizziness
Vestibular System Overview:
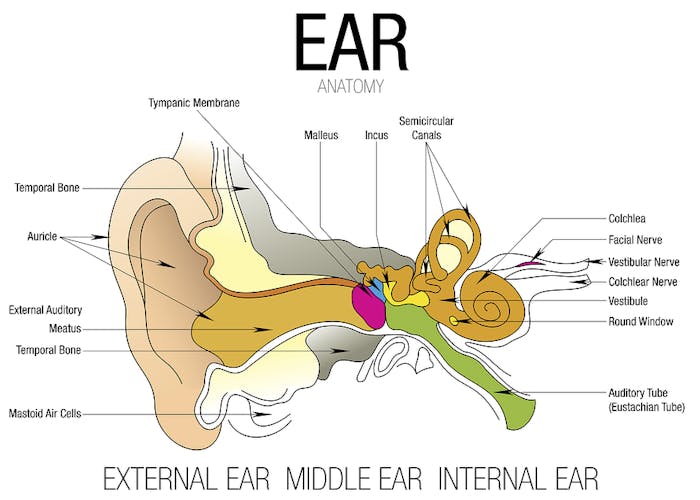
The vestibular system includes two pairs of 3 semicircular canals, the utricle and saccule. These components of the inner ear contribute to balance and equilibrium. Balance is controlled by an interrelationship of the vestibular system in the inner ear, your vision, proprioception, (balance sensors in your muscles, skin and joints and the brains interpretation of all the sensory input. The vestibular system allows you to see clearly while your head and body is moving. This is controlled via the vestibular ocular reflex.
All the sensory information coming into the brain needs to match and make sense to your brain. For example the semicircular canals in your ears may report to your brain that your are rotating your head to the right, your eyes send the same visual message and the receptors in the joints in your neck also inform your brain of similar information. If the brain receives conflicting information from any incoming sensory system it can leave you feeling dizzy, unsteady or disoriented. One example of a sensory conflict is when you are driving and stop at a traffic light. At the moment when you are still your vestibular system in your ear tells your brain you are not moving but when the bus next to you starts to travel forward before you do, your eyes tell your brain you are moving backwards. This conflict of sensory information can make you feel dizzy, off balance or make you feel like you are moving in the opposite direction. This may cause a knee jerk reaction of you slamming on your brakes. Another example is when you have an ear infection in one of the vestibular nerves. Both ears should produce matching sensory information going to your brain. When there is an infection, vascular insult or damage to one vestibular organ the information between the ears is unequal and your brain may interpret this mismatch as a sense of imbalance, dizziness, vertigo or spinning sensation.
Dizziness and Vertigo
These are sensations that you or your world is spinning when you are actually still. Everyone experiences dizziness and vertigo differently. Some people describe vertigo as an abnormal sense of motion of oneself or the environment. Others experience nausea, abnormal eye movements, lightheadedness, unsteadiness or complain they feel as if they are being pulled to one direction when walking or sitting.
Types of Vestibular Disorders:
There are many different vestibular disorders that can cause symptoms of imbalance, vertigo and dizziness. Below is a list of a few common vestibular disorders, including a brief description and common symptoms associated with each of them.
1. Benign Paroxysmal Positional Vertigo, BPPV
BPPV is the most common type of vestibular disorder. According to Ator GA, eighty percent of people aged 65 years old and older experienced dizziness and BPPV. BPPV is caused when otoconia also known as inner ear rocks or crystals break lose from the utricle, a vestibular organ and begin to move in the semicircular canals. When these rocks move in the canals they stimulate the ear’s hair cells and can cause brief episodes, (seconds) of mild to severe vertigo, spinning and imbalance. These symptoms of vertigo may reoccur whenever you move your head in a particular direction associated with the anatomical angle of the semicircular canal. Due to the effects of gravity and position, the most common type of BPPV involves the posterior canal.
2. Vestibular Neuritis & Labyrinthitis
These conditions are caused by inflammation, infection, or swelling of one or both of the vestibular nerves in the inner ear, this causes an imbalance of sensory input and hence vertigo. Vestibular neuritis and labrynthitis cause symptoms of imbalance and vertigo but labyrinthitis can also cause hearing loss and ringing in one’s ear. Symptoms usually come on very suddenly and cause severe vertigo, spinning, nausea and imbalance. The acute symptoms are usually constant and last for days and gradually decrease over the next few weeks. During the sub-acute and chronic stages the vertigo is usually brief and fleeting and may be brought on by head movements. Symptoms vary from person to person.
3. Meniere’s disease
This is a disorder of the entire inner ear causing repeat episodes of vertigo, fluctuating hearing loss, ear pressure, tinnitus (ringing in the ear) nausea, vomiting and falls. Attacks typically last for 2-4 hours and result in extreme fatigue for hours. The frequency and severity of episodes vary from patient to patient. The symptoms of Meniere’s disease occur from a build up of fluid in the ear. The cause is unknown but there are many theories regarding the etiology including: viral infections, genetic, and autoimmune deficits. People usually feel fine between attacks but may be left with a gradual decrease in hearing loss after each reoccurring attack.
4. Peri-lymphatic Fistula
Peri-lymphatic Fistula is a tear in the membrane of the oval window that divides the inner ear from the middle ear. When the tear occurs the specific fluid called perilymph fluid leaks from the inner ear into the middle ear. Symptoms from this disorder can be vertigo, hearing loss, and ear pressure. Possible causes of fistulas can be from some type of head trauma, childbirth or drastic changes in atmospheric pressure during airplane travel or scuba diving.
5. Superior or Anterior Canal Dehiscenc
This is a vestibular disorder caused by a small hole or defect in the ear bone of the superior, also called the anterior semicircular canal. This defect can be caused from a genetic or developmental defect. Symptoms of superior canal dehiscence can include dizziness, ear fullness or hearing loss. Due to the hole in the ear bone many patients complain that they can hear their own heart beat. Other symptoms may be dizziness and abnormal eye movements called nystagmus. Nystagmus is triggered by loud noises or by talking on a telephone. Sound induced dizziness is called the Tullio phenomenon. Some patients do not have any symptoms at all.
6. Acoustic Neuroma, also called Vestibular Schwannoma
Vestibular Schwannoma is a slow growing benign tumor of the cochlear (hearing) nerve. This tumor can cause the following symptoms: hearing loss, tinnitus, vertigo, imbalance, numbness weakness of the muscles of the face and gait disturbances. Since the tumor is slow growing, symptoms develop gradually and are not usually evident until the age of 30 or later. Usually a patient will complain of hearing issues prior to symptoms of vertigo and imbalance.
7. Vestibular Migraine
This is a condition similar to a migraine headache with or without the actual headache. Scientists are not completely sure of the etiology of the condition but they believe it is a constriction of the walls of the blood vessels around the brain. In a vestibular migraine the restriction is to the vestibular portion of the brain. Those suffering from a vestibular migraine usually have an aura or warning before the attack. Symptoms may be similar to a migraine headaches including sensitivity to bright lights, loud noises, motion and stimulating surroundings. Those suffering from vestibular migraines may also have symptoms of vertigo, imbalance, floating sensation, unsteadiness and dizziness. Again, symptoms vary from patient to patient.
- https://neurology.about.com/od/Symptoms/a/Vestibular-Migraine.htm
- https://www.neuropt.org/docs/vsig-english-pt-fact-sheets/migraine-associated-dizziness.pdf?sfvrsn=2
8. Concussion
Concussion is a mild traumatic brain injury caused by a blow to the head or body. Symptoms vary dramatically from person to person. Concussions can lead to a loss of consciousness, a bad headache, changes in alertness, irritability, sleep disturbances, nausea, vomiting, loss of memory or amnesia. Some people don’t develop any symptoms and others have vestibular symptoms such as dizziness, vertigo and imbalance
9. Other causes of vertigo
Other causes of vertigo or imbalance can be from cardiovascular disorders, central nervous system problems such as stroke (CVA), Parkinson’s disease and or Multiple Sclerosis. It is vital to have a doctor evaluate and diagnose your condition specifically so that the appropriate treatment can be employed. As you can see, multiple types of vestibular disorders have similar symptoms and vary from patient to patient. A thorough evaluation from an experienced vestibular medical specialist is vital.
Treatment:
Vestibular Rehabilitation consists of a systematic subjective and clinical evaluation by a physical or occupational therapist. A vestibular evaluation consists of completing comprehensive questionnaires revealing your medical history, symptoms and triggers. An in-depth clinical exam will be performed testing your balance, gait, and specific vestibular systems. Positional testing will be performed to assess the existence of benign paroxysmal positional vertigo BPPV or presence of otoconia-ear crystals in your semicircular canals. Position and motion sensitivity will also be evaluated. The goal is to localize the specific cause and impairments involved in your vestibular dysfunction.
Our clinic may further evaluate and treat your vestibular dysfunction with the use of video frenzel lenses. These video goggles are used to evaluate and record your eye movements to see how your eyes respond to various body positions and specific head movements. These recording help to better visualize and isolate the cause of your vestibular dysfunction, track progress and assists us to choose the most appropriate treatment course for your individual condition and deficits.
After your physical therapist performs a vestibular evaluation, weekly treatment sessions will include specific exercises, functional training and education geared toward your individual deficits. The goals are to restore balance, improve gait and function, establish clear vision with head motion, desensitize motion-provoked dizziness, and reduce your anxiety, fear and your risk of falling. Treatments may include but are not limited to:
- Canalithe repositioning, or Epley Maneuver
- Gaze stabilization exercise
- Substitution exercises
- Static and dynamic balance exercise
- Gait Training with and without head movements
- Home safety modifications
- Strength and Endurance exercise
- Specific functional activities geared toward your particular deficits: ie trips to the grocery store, walking on uneven surfaces, walking in open spaces, walking in the dark…
For further detailed information on vestibular dysfunctions, references, diagnostic testing, appropriate treatment options, patient information sheets or support group information see the list of links to other vestibular and medical websites.
- https://vestibular.org
- https://www.neuropt.org/docs/vsig-english-pt-fact-sheets/common-vestibular-tests-performed.pdf?sfvrsn=2
- https://www.neuropt.org/special-interest-groups/vestibular-rehabilitation/patient-education-fact-sheets
- https://www.american-hearing.org/disorders/central/migraine/mav.html
- https://www.dizziness-and-balance.com
- https://newsinhealth.nih.gov/issue/aug2012/feature1



